Introduction
Little has been published on the sensation felt in the urethra during voiding, and most studies are from several decades ago.
We studied the urethral voiding sensation in a series of young healthy men, recruited in the community. We also evaluated if visual and audible impulses can have an influence on the sensations during the voiding process.
Materials and Methods
After approval by the local ethics committee, 10 healthy male volunteers where recruited by advertisement. If urological and neurologic history was negative, and a control uroflowmetry at arrival was reported by the participants as being “normal, as in daily life”, a residual was measured with ultrasonography. Participants read the study protocol and signed an informed consent.
Non invasive uroflowmetry was done 2 times on a Type AQTT uroflowmeter (Laborie Medical Technologies Europe) [
1]. Normal desire to void was required to start both tests.
A first test uroflowmetry (UROFLOW 1) was done with visual and audible observation possible. For the second test uroflowmetry (UROFLOW 2) participants wore a blindfold eye patch (3M, Opticlude orthopedic eye patch for occlusion therapy) and earcups plus earplugs (Adulte Amplivox auralgard II), blocking visual and audible signals completely. Between tests free drinking was made available (water or soft drinks). All uroflowmetries were done in the sitting position to avoid concern to miss the flowmeter when blinded.
Reporting start and stop of outflow was noted on the curve. Sensation was evaluated after UROFLOW 1 and 2 with scoring “very clearly, clearly, moderate, uncertain/negative” of following statements: “ I could feel the start of the urine flow. I could feel the stop of the urine flow. I could feel urine passing through my urine canal. The passage of the urine stream felt warm”. It was also asked if another sensation had been felt and if affirmative to describe it.
SPSS 22 was used for statistical analysis. Answers are given with the number of participants. Descriptive data are given as median (min-max). P-values are based on Wilcoxon signed rank test in ordinal and scale variables, Mc Nemar test for yes/no questions. Correlations were done with Spearman rho correlation test.
Results
The volunteers had age 27,5 (23 to 34) years; weight 72 (65 to 87) kg; length 182 (169 to 187) cm. All reported the uroflowmetry at arrival as normal for their daily life. Postvoid residual was absent in 8 while two had residue of 9 ml and 10 ml.
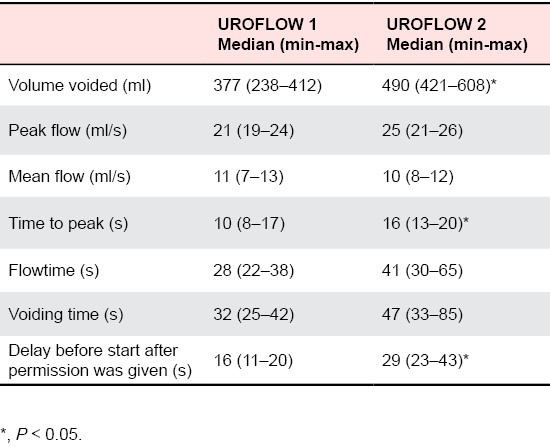
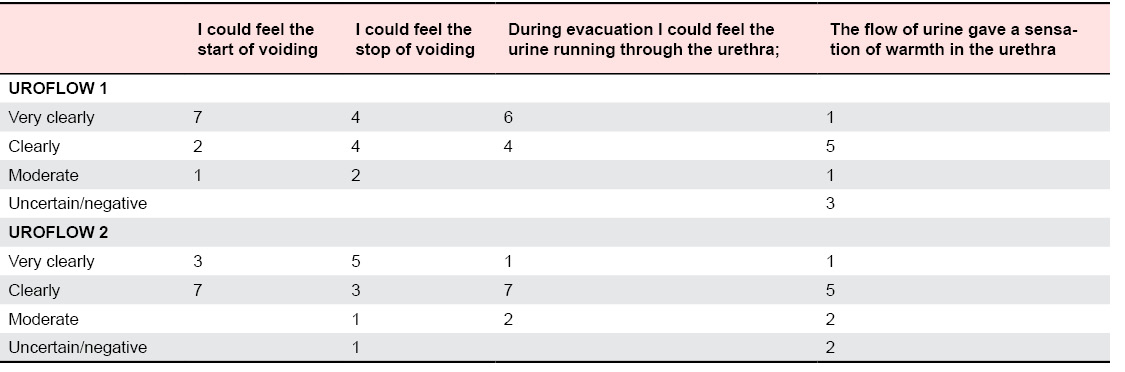
The results of the uroflowmetries are given in Table 1. The sensations reported are given in Table 2.
The uroflowmetry curve was of bell shape (7/10 in UROFLOW 1 and 5/10 in UROFLOW 2 ) or shape with important peaks (3/10 in UROFLOW 1 and 5/10 in UROFLOW 2) [
1]. In 2 participants a change from bell shape to shape with peaks was seen between UROFLOW 1 and 2. However this last pattern was also noted on the uroflow at arrival and thus was considered as a normal variation.
Reporting stop of the urine outflow while the stream was still running was done by 1 on UROFLOW 1 and by 4 on UROFLOW 2. Two reported stop of the outflow after it had stopped already in UROFLOW 1. In UROFLOW 2 one participant was uncertain if voiding had started when urine was passing.
Three participants reported other sensations during uroflowmetry. Participant N° 6 reported a sensation as of slow building up of the stream (UROFLOW 1) and somewhat lowered stream (UROFLOW 2) though his flow parameters were not different from those of the whole group. Participant N° 8 reported a very relaxed feeling (UROFLOW 1) and tingling calves (UROFLOW 2). Participant N° 9 reported a “not normal sensation as in daily life” during the first test, while no such sensation was reported after UROFLOW 2.
There was no significant correlation between scoring of the statements and uroflowmetry parameters, between time before outflow started and the volume voided, and between the data of UROFLOW 1 and 2, which permits to exclude in this series a clear influence of different flow parameters on the sensations reported.
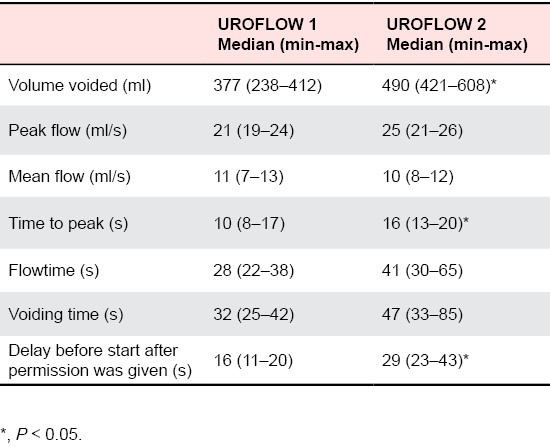
Table 1. Data from the uroflowmetries.
Discussion
Reporting on sensations elicited by activities happening inside the body is by definition subjective and a result of interpretation of sensory impulses reaching consciousness. What is felt and how it is reported is most probably the result of a very complex process: minute observation of one’s own sensation, ease and correctness of expression, psychological and environmental influences. The special sensations reported by 3 participants can illustrate this. What is felt will also depend on input from non- related organs.
That relationship exists between urethral afferents and micturition or bladder function has been shown before in different ways. Involvement of urethral sensory information in desire to void is suggested by the fact that strong desire to void at full bladder is localized very low in the pelvis and urethra, probably related to an increase of intra-urethral pressure at the sphincter level [
2]. Various forms of stimulation of the urethra (as introducing a cystoscope or catheter) can cause a desire to void, indicating that estimating that the bladder is full may depend on bladder a
nd on urethral afferent impulses [
3]. Studies in patients with different lesions of the innervation showed that these afferent potentials run in the pudendal nerves, and can create a sensation of passing urine [
4], of pain, temperature and touch [
5]. Anesthetic blocking of urethral afferents can lead to incomplete bladder emptying and the need to strain in healthy volunteers [
6]. Sensations occurring with the introduction of a catheter are usually described as similar to those at the onset of micturition, but after 10 or 15 seconds the sensation fades away and patients are then unaware of the catheter within the posterior urethra. This would imply that receptors which have responded to change of stretch adapt to the increased urethral diameter [
7]. As the sensation of passage of urine continues during flow such adaptation of receptors involved in flow sensation seems unlikely. In this study we found no correlation between different flow parameters as voided volume, peak flow and flow time and the level or type of sensation reported. What would happen if flow was done under more extreme circumstances, as after holding urine beyond strong desire to void, remains to be studied.
The knowledge of neurophysiological structures related to sensation in the urethra is more limited than the data on bladder [
8]. Histologically in the proximal urethra a transition to a stratified or columnar epithelium accompanied by a lack of urothelial-specific differentiation markers and microvilli on the apical surface has been described [
9]. The urethral epithelium is part of a signaling system involving projections of the neuroendocrine cells, interstitial cells and sensory nerve endings. George and Dixon [
10] described an extensive plexus of nerve fibers throughout the lamina propria and densest immediately beneath the epithelial lining. These are believed to sub serve a sensory function. Specialized sensory endings as found within striated muscle (
i.e. muscle spindles) do not occur in the external urethral sphincter [
11]. Flow receptors running through the pudendal nerve were suggested by Todd [
12].
Histological studies have also shown that the pathways conducting impulses subserving pain and temperature from the urethra run in the same region as that conducting impulses subserving the sensation of full bladder and pain of the bladder [
4]. If the spino-thalamic tract is divided, patients might still feel sensation that micturition is impending, that it is progressing, that it has ceased. These sensations would therefore be due to impulses arising in the urethral mucosa, in the urethral sphincter and the perineal muscles that act synergically with the sphincter. Impulses from these structures travel via the posterior columns [
5].
In standardized conditions as in our pilot study, healthy young participants declare feeling passage of urine either very clearly or clearly. Nathan [
5] proposed 3 components in sensation that urine is passing: an awareness of the opening of the sphincter musculature, a feeling of something passing along the urethra and a thermal sensation. Nathan described sensation of urine passage as only a slight sensation, but in focused young men in study conditions as we had, it becomes much more clear. Thermal sensation, as studied by Nathan [
13] was reported by 7/10 and 8/10 of our participants during UROFLOW 1 and UROFLOW 2 respectively. If diagnosing a deficiency of urethral sensation can be an indication of unknown neurologic pathology, as was found in bladder filling sensation [
14], needs more research.
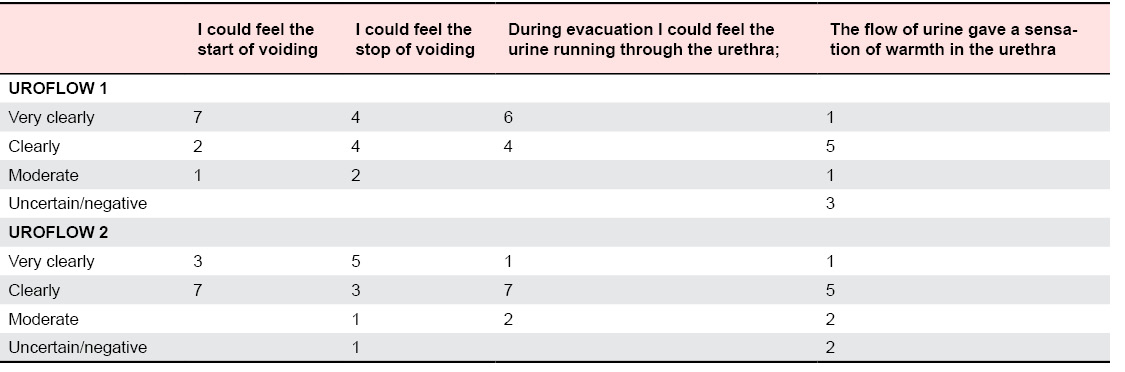
Table 2. The grading of sensation statements after UROFLOW 1 and 2 (number of participants).
That urethral sensation can be influenced by keeping the eyes closed was mentioned by Nathan in one male patient [
5]. When visual
ánd audible signals were completely blocked many of our participants found that sensation of passage of urine became less clear. We also noted that voiding took a significant longer time to start, and the feeling that flow had started had become less reliable. Sensation of warmth was independent of blocking visual and audible observation. One can hypothesize that when men during voiding look at the stream and hear the running of the urine in the toilet such extra input can influence the overall sensation related to micturition and the estimation when the stream starts and stops. Such influence will vary between subjects, as we have seen in our study.
Although our study group consists of a well confined sample and our investigation technique was standardized, there are limitations to our observations: the series is small, all participants are men. As all uroflowmetries were done in the sitting position to avoid concern for missing the uroflowmeter, we have no information on the urethral sensation of urine flow in standing position. Each evaluation was done on only one uroflowmetry as this seemed sufficient for studying reporting of sensation. It needs to be evaluated if repeated uroflowmetry would give a different result.
Despite the shortcomings we think that our data bring attention to different aspects of the complex process involved in urethral sensation during voiding, as the type and level of sensation, the influence of visual and audible information, the independence of normal flow volume and speed. More observations are needed, in larger groups of participants, of different age, different gender, and with well-defined pathologies to enlarge the clinical picture and better determine the diagnostic value of such sensory evaluation.
Conclusion
All young healthy men participating in this study reported urethral sensation during voiding. The sensation was independent of the uroflowmetry parameters. Blocking visual and audible information had an influence on the sensory function and the voiding, indicating the complexity of sensation and its interpretation.