Increased utilization of external beam radiotherapy relative to cystectomy for localized, muscle-invasive bladder cancer: a SEER analysis

Objective: To assess recent utilization patterns of radiotherapy (RT) relative to cystectomy for muscle-invasive bladder cancer (MIBC) and evaluate survival trends over time in patients receiving RT.
Materials and Methods: The surveillance, epidemiology, and end results program (SEER) was used to identify patients diagnosed between 1992 and 2013 with localized MIBC. Patients with a prior history of non-bladder malignancy, who received no treatment, or did not have available treatment information, were excluded. Treatment utilization patterns were assessed using Cochran-Armitage tests for trend, and patient characteristics were compared using chi-square tests. Overall survival (OS) and cause-specific survival (CSS) were estimated using the Kaplan-Meier method. All-cause (ACM) and cause-specific mortality (CSM) were evaluated with multivariable Cox proportional hazards regression.
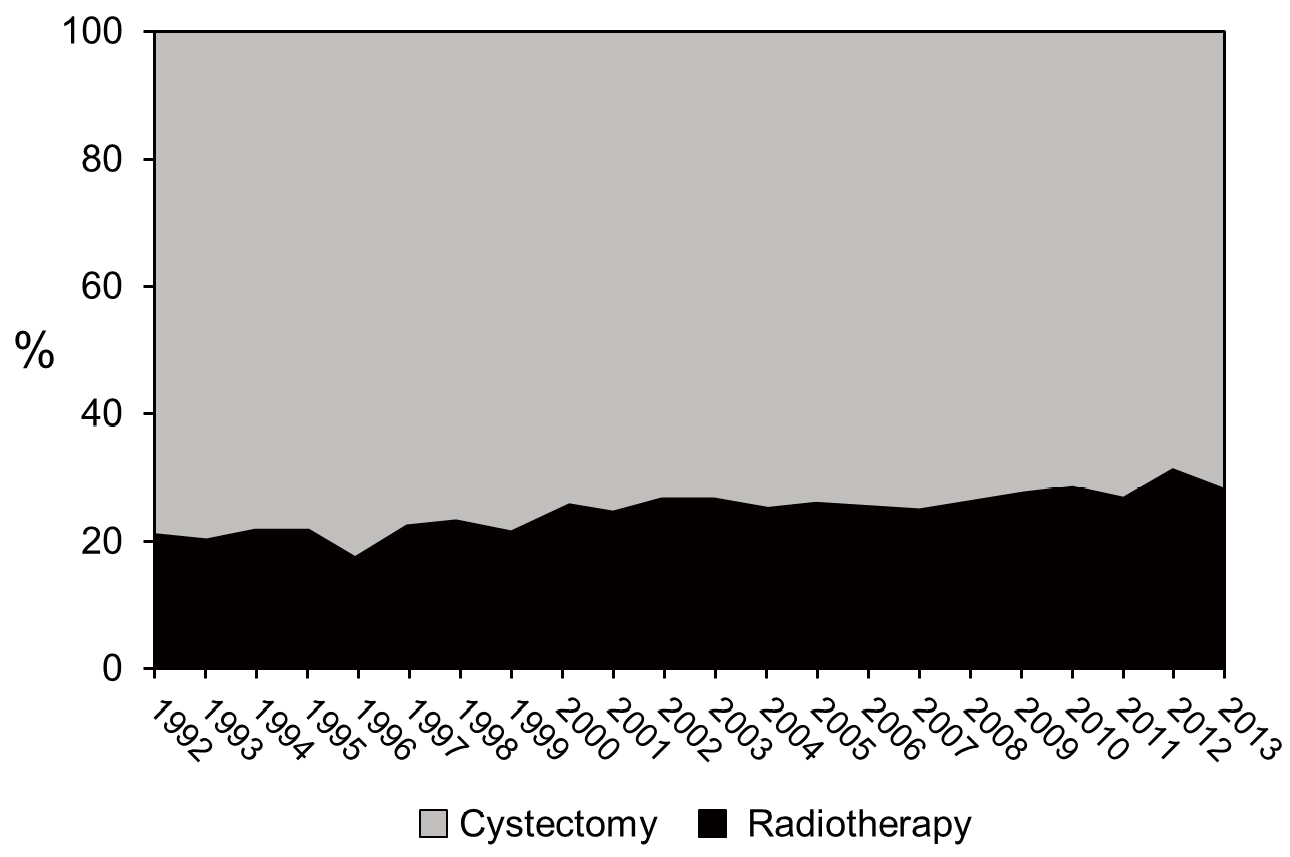
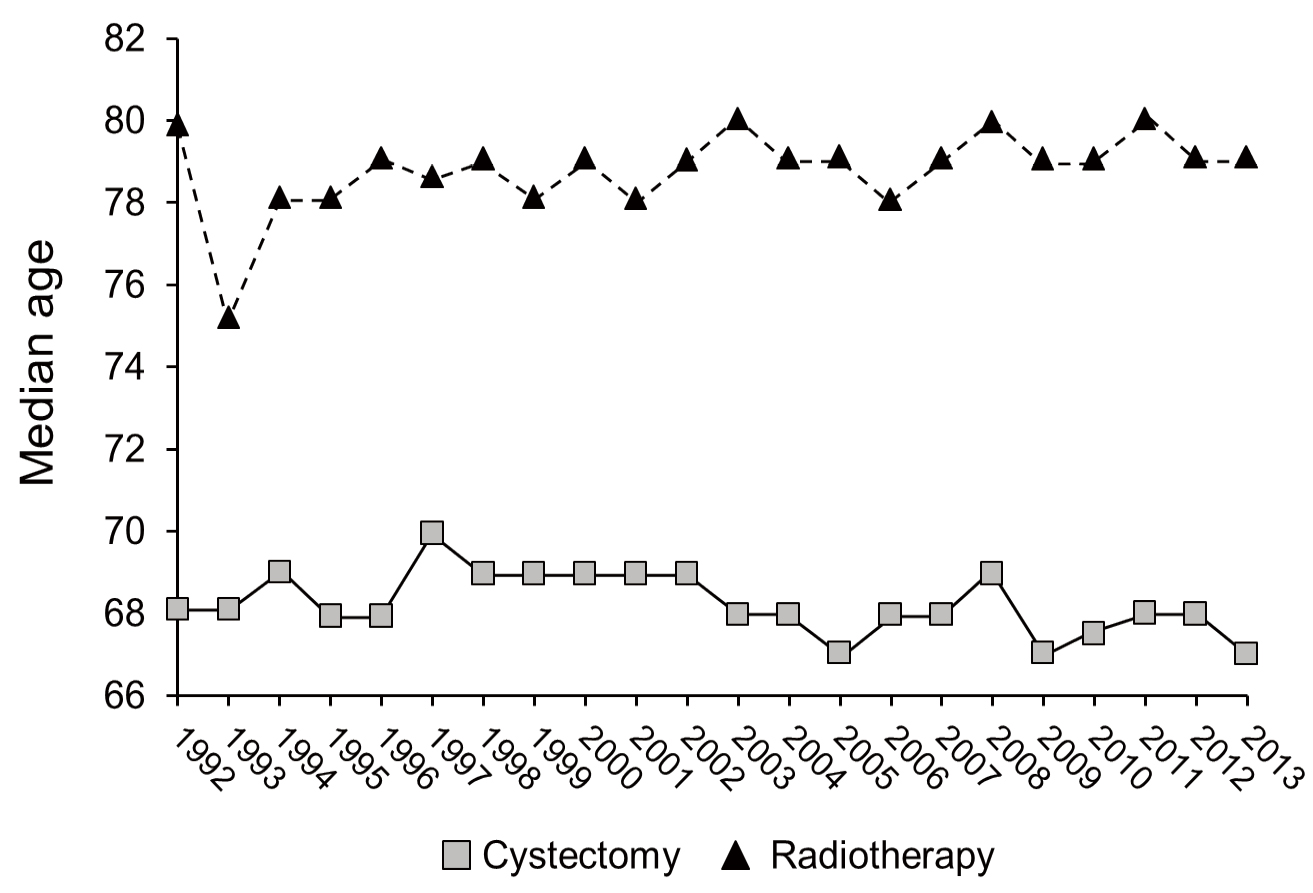
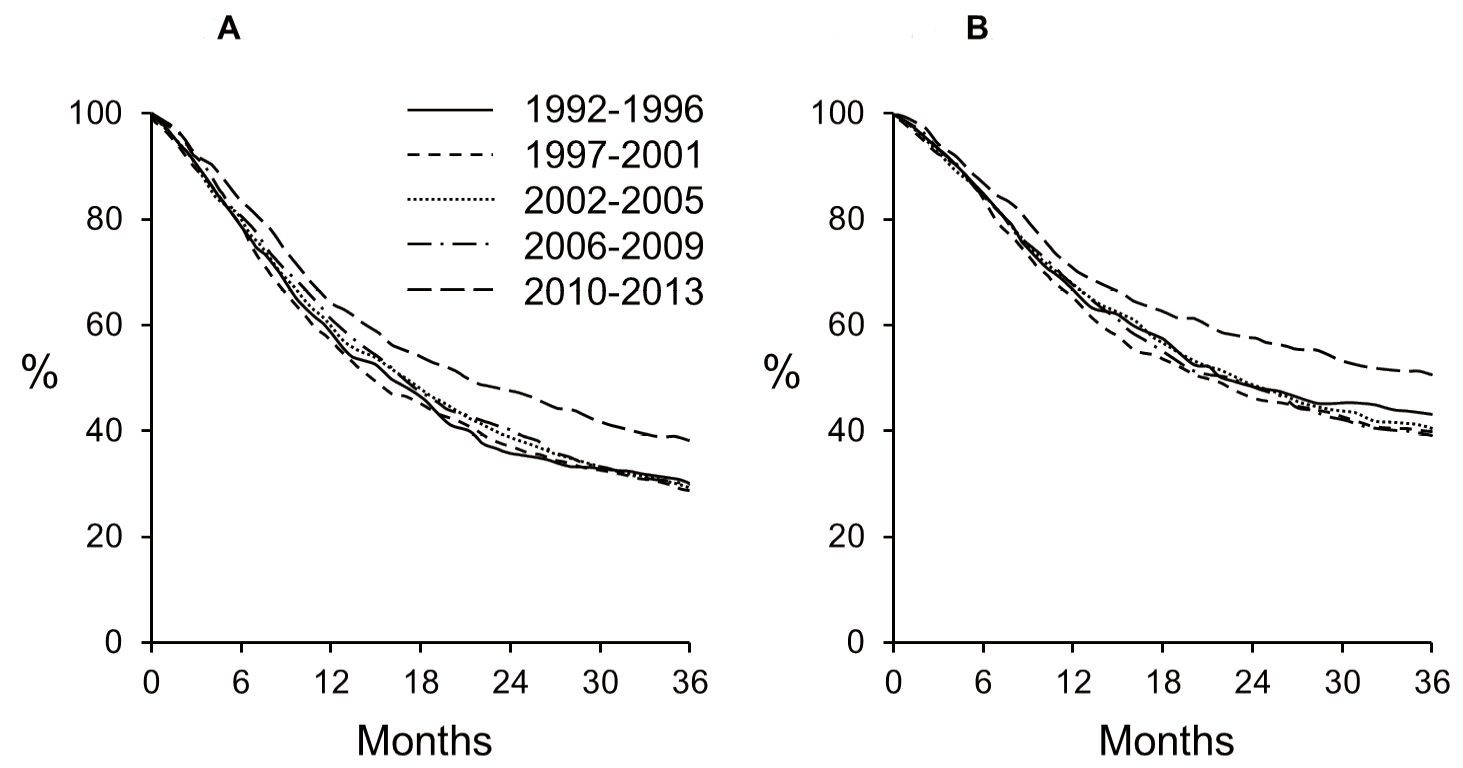
Results: Of 16175 patients analyzed, 11917 (74%) underwent cystectomy, and 4258 (26%) were treated with RT. Patients who received RT were older (median age 79 vs. 68, P < 0.01). Over time, the proportion of patients receiving RT relative to cystectomy increased (24% 1992–2002 vs. 28% 2003–2013, P < 0.01), despite median patient age throughout the study period remaining unchanged (71 for each 1992–2002 and 2003–2013, P = 0.41). For RT, compared with patients diagnosed earlier, those diagnosed from 2010–2013 showed improved OS (64% vs. 60% at 1 year, P < 0.01; 38% vs. 29% at 3 years, P < 0.01) and CSS (71% vs. 67% at 1 year, P = 0.01; 51% vs. 40% at 3 years, P < 0.01). On multivariable analysis, diagnosis from 2010–2013 was associated with a lower estimated risk of ACM (hazard ratio 0.77; 95% confidence interval 0.66–0.89, P < 0.001) and CSM (hazard ratio 0.81; 95% confidence interval 0.67–0.97, P = 0.02).
Conclusion: Utilization of RT for localized MIBC increased relative to cystectomy from 1992 to 2013, despite the median age of treated patients remaining unchanged. More recent survival outcomes for patients receiving RT were improved, supporting continued use of bladder preservation strategies utilizing RT.
Introduction
Materials and Methods
Study population and study design
Statistical analyses
Results
Patient characteristics
Utilization of RT over time
Overall and cause-specific survival with RT
| Characteristic | No. of patients (%) | Radiotherapy (%) | Cystectomy (%) | P value* | |
|---|---|---|---|---|---|
| Total | 16175 (100) | 4258 (26.3) | 11917 (73.6) | < 0.0001 | |
| Age (years) | < 0.0001 | ||||
| 21–50 | 836 (5.2) | 67 (8.0) | 769 (92.0) | ||
| 50–59 | 2311 (14.3) | 253 (10.9) | 2058 (89.1) | ||
| 60–69 | 4346 (26.9) | 645 (14.8) | 3701 (85.2) | ||
| 70–79 | 5130 (31.7) | 1292 (25.2) | 3838 (74.8) | ||
| 80–89 | 3191 (20.3) | 1726 (54.1) | 1465 (45.9) | ||
| ≥ 90 | 361 (2.2) | 275 (76.2) | 86 (23.8) | ||
| Sex | < 0.0001 | ||||
| Male | 11781 (72.8) | 2974 (25.2) | 8807 (74.8) | ||
| Female | 4394 (27.2) | 1284 (29.2) | 3110 (70.8) | ||
| Race | < 0.0001 | ||||
| White | 13488 (83.4) | 3524 (26.1) | 9964 (73.9) | ||
| Hispanic | 860 (5.3) | 192 (22.3) | 668 (77.7) | ||
| Black | 1046 (6.5) | 357 (34.1) | 689 (65.9) | ||
| Asian or Pacific Islander | 701 (4.3) | 168 (24.0) | 533 (76.0) | ||
| Other or unknown | 80 (0.4) | 17 (21.2) | 63 (78.8) | ||
| Marital status | < 0.0001 | ||||
| Single | 1680 (10.4) | 413 (24.6) | 1267 (75.4) | ||
| Married | 9802 (60.6) | 2185 (22.3) | 7617 (77.7) | ||
| Separated | 146 (0.9) | 27 (18.5) | 119 (81.5) | ||
| Divorced | 1387 (8.6) | 324 (23.4) | 1063 (76.6) | ||
| Widowed | 2664 (16.5) | 1167 (43.8) | 1497 56.2) | ||
| Unmarried or domestic partner | 8 (0.05) | 3 (37.5) | 5 (62.5) | ||
| Unknown | 488 (3.0) | 139 (28.5) | 349 (71.5) | ||
| Tumor differentiation | < 0.0001 | ||||
| Well | 157 (1.0) | 29 (18.5) | 128 (81.5) | ||
| Moderately | 1165 (7.2) | 237 (20.3) | 928 (79.7) | ||
| Poorly | 6828 (42.2) | 1796 (26.3) | 5032 (73.7) | ||
| Undifferentiated | 7442 (46.0) | 1988 (26.7) | 5454 (73.3) | ||
| Histology | < 0.0001 | ||||
| Urothelial cell carcinoma | 14895 (92.1) | 4038 (27.1) | 10857 (72.9) | ||
| Squamous cell carcinoma | 779 (4.8) | 169 (21.7) | 610 (78.3) | ||
| Adenocarcinoma | 501 (3.1) | 51 (10.2) | 450 (89.8) | ||
| Stage | < 0.0001 | ||||
| T2 | 9219 (57.0) | 3245 (35.2) | 5974 (64.8) | ||
| T3 | 6000 (37.1) | 784 (13.1) | 5216 (86.9) | ||
| T4 | 956 (5.9) | 229 (24.0) | 727 (76.0) | ||
| Variable | HR (95% CI) | P value | |
|---|---|---|---|
| Age (years) | |||
| 21–49 | 1.00 (ref) | ||
| 50–59 | 1.21 (0.84–1.74) | 0.309 | |
| 60–69 | 1.55 (1.10–2.20) | 0.013 | |
| 70–79 | 2.31 (1.65–3.25) | < 0.001 | |
| 80–89 | 2.86 (2.04–4.01) | < 0.001 | |
| ≥ 90 | 3.96 (2.7565.69) | < 0.001 | |
| Sex | |||
| Female | 1.00 (ref) | ||
| Male | 0.98 (0.90–1.07) | 0.627 | |
| Race | |||
| White | 1.00 (ref) | ||
| Hispanic | 0.94 (0.78–1.13) | 0.527 | |
| Black | 1.22 (1.06–1.39) | 0.004 | |
| Asian | 0.84 (0.69–1.02) | 0.077 | |
| Other or unknown | 0.92 (0.47–1.77) | 0.791 | |
| Marital status | |||
| Married | 1.00 (ref) | ||
| Single | 1.24 (1.09–1.42) | 0.002 | |
| Separated | 1.26 (0.82–1.94) | 0.302 | |
| Divorced | 1.35 (1.16–1.57) | < 0.001 | |
| Widowed | 1.04 (0.94–1.14) | 0.448 | |
| Unmarried | 1.07 (0.15–7.64) | 0.947 | |
| Unknown | 1.15 (0.93–1.43) | 0.187 | |
| Tumor differentiation | |||
| Well | 1.00 (ref) | ||
| Moderately | 1.30 (0.83–2.06) | 0.255 | |
| Poorly | 1.23 (0.79–1.90) | 0.357 | |
| Undifferentiated | 1.20 (0.77–1.85) | 0.419 | |
| Unknown | 1.39 (0.87–2.20) | 0.165 | |
| Histology | |||
| Urothelial carcinoma | 1.00 (ref) | ||
| Adenocarcinoma | 0.85 (0.59–1.23) | 0.395 | |
| Squamous cell carcinoma | 1.38 (1.15–1.65) | < 0.001 | |
| Year of diagnosis | |||
| 1992 to 1996 | 1.00 (ref) | ||
| 1997 to 2001 | 1.01 (0.88–1.15) | 0.936 | |
| 2002 to 2005 | 0.98 (0.86–1.12) | 0.777 | |
| 2006 to 2009 | 0.92 (0.80–1.05) | 0.207 | |
| 2010 to 2013 | 0.77 (0.66–0.89) | < 0.001 | |
| Stage | |||
| T2 | 1.00 (ref) | ||
| T3 | 1.08 (0.98-1.19) | 0.132 | |
| T4 | 1.38 (1.17-1.62) | <0.001 | |
Discussion
| Variable | HR (95% CI) | P value | |
|---|---|---|---|
| Age (years) | |||
| 21–49 | 1.00 (ref) | ||
| 50–59 | 1.31 (0.86–1.98) | 0.207 | |
| 60–69 | 1.33 (0.89–1.98) | 0.163 | |
| 70–79 | 1.75 (1.19–2.59) | 0.005 | |
| 80–89 | 2.23 (1.51–3.30) | < 0.001 | |
| ≥ 90 | 2.82 (1.86–4.29) | < 0.001 | |
| Sex | |||
| Female | 1.00 (ref) | ||
| Male | 0.86 (0.78–0.95) | 0.004 | |
| Race | |||
| White | 1.00 (ref) | ||
| Hispanic | 1.10 (0.89–1.35) | 0.390 | |
| Black | 1.31 (1.13–1.53) | < 0.001 | |
| Asian | 0.99 (0.79–1.24) | 0.913 | |
| Other or unknown | 0.82 (0.37–1.83) | 0.627 | |
| Marital status | |||
| Married | 1.00 (ref) | ||
| Single | 1.18 (1.01–1.38) | 0.041 | |
| Separated | 1.35 (0.82–2.22) | 0.241 | |
| Divorced | 1.35 (1.13–1.61) | < 0.001 | |
| Widowed | 0.95 (0.85–1.07) | 0.423 | |
| Unmarried | 1.34 (0.19–9.57) | 0.774 | |
| Unknown | 1.16 (0.91–1.49) | 0.237 | |
| Tumor differentiation | |||
| Well | 1.00 (ref) | ||
| Moderately | 1.19 (0.70–2.02) | 0.517 | |
| Poorly | 1.19 (0.72–1.97) | 0.489 | |
| Undifferentiated | 1.15 (0.70–2.02) | 0.576 | |
| Unknown | 1.41 (0.83–2.39) | 0.206 | |
| Histology | |||
| Urothelial carcinoma | 1.00 (ref) | ||
| Adenocarcinoma | 0.76 (0.48–1.19) | 0.231 | |
| Squamous cell carcinoma | 1.34 (1.08–1.66) | 0.008 | |
| Year of diagnosis | |||
| 1992 to 1996 | 1.00 (ref) | ||
| 1997 to 2001 | 1.09 (0.92–1.29) | 0.348 | |
| 2002 to 2005 | 1.02 (0.87–1.21) | 0.809 | |
| 2006 to 2009 | 1.03 (0.87–1.23) | 0.699 | |
| 2010 to 2013 | 0.81 (0.67–0.97) | 0.021 | |
| Stage | |||
| T2 | 1.00 (ref) | ||
| T3 | 1.13 (1.01–1.28) | 0.036 | |
| T4 | 1.57 (1.31–1.88) | < 0.001 | |
-
-
American Cancer Society (2017) Cancer Facts & Figures 2017. Atlanta: American Cancer Society. Available from: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2017.html [Google Scholar]
-
Kaufman DS, Shipley WU, Feldman AS (2009) Bladder cancer. Lancet 374: 239-249. doi: https://doi.org/10.1016/S0140-6736(09)60491-8. [View Article] [PubMed] [Google Scholar]
-
Grossman HB, Natale RB, Tangen CM, Speights VO, Vogelzang NJ, et al. (2003) Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N Engl J Med 349: 859-866. doi: https://doi.org/10.1056/NEJMoa022148. [View Article] [PubMed] [Google Scholar]
-
Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, et al. (2001) Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol 19: 666-675. doi: https://doi.org/10.1200/JCO.2001.19.3.666. [View Article] [PubMed] [Google Scholar]
-
Zehnder P, Studer UE, Skinner EC, Dorin RP, Cai J, et al. (2011) Super extended versus extended pelvic lymph node dissection in patients undergoing radical cystectomy for bladder cancer: a comparative study. J Urol 186: 1261-1268. doi: https://doi.org/10.1016/j.juro.2011.06.004. [View Article] [PubMed] [Google Scholar]
-
Shabsigh A, Korets R, Vora KC, Brooks CM, Cronin AM, et al. (2008) Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol 55: 164-174. doi: https://doi.org/10.1016/j.eururo.2008.07.031. [View Article] [PubMed] [Google Scholar]
-
Rödel C, Grabenbauer GG, Kühn R, Papadopoulos T, Dunst J, et al. (2002) Combined-modality treatment and selective organ preservation in invasive bladder cancer: long-term results. J Clin Oncol 20: 3061-3071. doi: https://doi.org/10.1200/JCO.2002.11.027. [View Article] [PubMed] [Google Scholar]
-
James ND, Hussain SA, Hall E, Jenkins P, Tremlett J, et al. (2012) Radiotherapy with or without chemotherapy in muscle-invasive bladder cancer. N Engl J Med 366: 1477-1488. doi: https://doi.org/10.1056/NEJMoa1106106. [View Article] [PubMed] [Google Scholar]
-
Kaufman DS, Shipley WU, Griffin PP, Heney NM, Althausen AF, et al. (1993) Selective bladder preservation by combination treatment of invasive bladder cancer. N Engl J Med 329: 1377-1382. doi: https://doi.org/10.1056/NEJM199311043291903. [View Article] [PubMed] [Google Scholar]
-
Hagan MP, Winter KA, Kaufman DS, Wajsman Z, Zietman AL, et al. (2003) RTOG 97-06: initial report of a phase I-II trial of selective bladder conservation using TURBT, twice-daily accelerated irradiation sensitized with cisplatin, and adjuvant MCV combination chemotherapy. Int J Radiat Oncol Biol Phys 57: 665-672. doi: https://doi.org/10.1016/S0360-3016(03)00718-1. [View Article] [PubMed] [Google Scholar]
-
Kaufman DS, Winter KA, Shipley WU, Heney NM, Wallace 3rd, et al. (2008) Phase I-II RTOG study (99-06) of patients with muscle-invasive bladder cancer undergoing transurethral surgery, paclitaxel, cisplatin, and twice-daily radiotherapy followed by selective bladder preservation or radical cystectomy and adjuvant chemotherapy. Urology 73: 833-837. doi: https://doi.org/10.1016/j.urology.2008.09.036. [View Article] [PubMed] [Google Scholar]
-
Mak RH, Hunt D, Shipley WU, Efstathiou JA, Tester WJ, et al. (2014) Long-term outcomes in patients with muscle-invasive bladder cancer after selective bladder-preserving combined-modality therapy: a pooled analysis of Radiation Therapy Oncology Group protocols 8802, 8903, 9506, 9706, 9906, and 0233. J Clin Oncol 32: 3801-3809. doi: https://doi.org/10.1200/JCO.2014.57.5548. [View Article] [PubMed] [Google Scholar]
-
Kozak KR, Hamidi M, Manning M, Moody JS (2012) Bladder preservation for localized, muscle-invasive bladder cancer: the survival impact of local utilization rates of definitive radiotherapy. Int J Radiat Oncol Biol Phys 83: 197-204. doi: https://doi.org/10.1016/j.ijrobp.2011.12.038. [View Article] [PubMed] [Google Scholar]
- Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) Research Data (1973-2014), National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2018, based on the November 2017 submission
-
Giacalone NJ, Shipley WU, Clayman RH, Niemierko A, Drumm M, et al. (2017) Long-term Outcomes After Bladder-preserving Tri-modality Therapy for Patients with Muscle-invasive Bladder Cancer: An Updated Analysis of the Massachusetts General Hospital Experience. Eur Urol 71: 952-960. doi: https://doi.org/10.1016/j.eururo.2016.12.020. [View Article] [PubMed] [Google Scholar]
-
Efstathiou JA, Spiegel DY, Shipley WU, Heney NM, Kaufman DS, et al. (2011) Long-term outcomes of selective bladder preservation by combined-modality therapy for invasive bladder cancer: the MGH experience. Eur Urol 61: 705-711. doi: https://doi.org/10.1016/j.eururo.2011.11.010. [View Article] [PubMed] [Google Scholar]
-
Mitin T, Hunt D, Shipley WU, Kaufman DS, Uzzo R, et al. (2013) Transurethral surgery and twice-daily radiation plus paclitaxel-cisplatin or fluorouracil-cisplatin with selective bladder preservation and adjuvant chemotherapy for patients with muscle invasive bladder cancer (RTOG 0233): a randomised multicentre phase 2 trial. Lancet Oncol 14: 863-872. doi: https://doi.org/10.1016/S1470-2045(13)70255-9. [View Article] [PubMed] [Google Scholar]
-
Zapatero A, Martin De Vidales, Arellano R, Ibañez Y, Bocardo G, et al. (2012) Long-term results of two prospective bladder-sparing trimodality approaches for invasive bladder cancer: neoadjuvant chemotherapy and concurrent radio-chemotherapy. Urology 80: 1056-1062. doi: https://doi.org/10.1016/j.urology.2012.07.045. [View Article] [PubMed] [Google Scholar]
-
Lagrange J, Bascoul-Mollevi C, Geoffrois L, Beckendorf V, Ferrero J, et al. (2010) Quality of life assessment after concurrent chemoradiation for invasive bladder cancer: results of a multicenter prospective study (GETUG 97-015). Int J Radiat Oncol Biol Phys 79: 172-178. doi: https://doi.org/10.1016/j.ijrobp.2009.10.038. [View Article] [PubMed] [Google Scholar]
-
Aizer AA, Wilhite TJ, Chen M, Graham PL, Choueiri TK, et al. (2014) Lack of reduction in racial disparities in cancer-specific mortality over a 20-year period. Cancer 120: 1532-1539. doi: https://doi.org/10.1002/cncr.28617. [View Article] [PubMed] [Google Scholar]
-
Aizer AA, Chen M, McCarthy EP, Mendu ML, Koo S, et al. (2013) Marital status and survival in patients with cancer. J Clin Oncol 31: 3869-3876. doi: https://doi.org/10.1200/JCO.2013.49.6489. [View Article] [PubMed] [Google Scholar]
-
Scosyrev E, Yao J, Messing E (2009) Urothelial carcinoma versus squamous cell carcinoma of bladder: is survival different with stage adjustment?. Urology 73: 822-827. doi: https://doi.org/10.1016/j.urology.2008.11.042. [View Article] [PubMed] [Google Scholar]
-
Huddart RA, Hall E, Lewis R, Birtle A (2010) Life and death of spare (selective bladder preservation against radical excision): reflections on why the spare trial closed. BJU Int 106: 753-755. doi: https://doi.org/10.1111/j.1464-410X.2010.09537.x. [View Article] [PubMed] [Google Scholar]
-
Gray PJ, Lin CC, Jemal A, Shipley WU, Fedewa SA, et al. (2014) Clinical-pathologic stage discrepancy in bladder cancer patients treated with radical cystectomy: results from the national cancer data base. Int J Radiat Oncol Biol Phys 88: 1048-1056. doi: https://doi.org/10.1016/j.ijrobp.2014.01.001. [View Article] [PubMed] [Google Scholar]
-
Kulkarni GS, Hermanns T, Wei Y, Bhindi B, Satkunasivam R, et al. (2017) Propensity score analysis of radical cystectomy versus bladder-sparing trimodal therapy in the setting of a multidisciplinary bladder cancer clinic. J Clin Oncol 35: 2299-2305. doi: https://doi.org/10.1200/JCO.2016.69.2327. [View Article] [PubMed] [Google Scholar]
-
Vashistha V, Wang H, Mazzone A, Liss MA, Svatek RS, et al. (2016) Radical cystectomy compared to combined modality treatment for muscle-invasive bladder cancer: a systematic review and meta-analysis. Int J Radiat Oncol Biol Phys 97: 1002-1020. doi: https://doi.org/10.1016/j.ijrobp.2016.11.056. [View Article] [PubMed] [Google Scholar]
-
National Cancer Institute (2017) Surveillance, Epidemiology, and End Results Program. Radiation/Chemotherapy Databases. Available from: https://seer.cancer.gov/data/treatment.html [Google Scholar]
-

